Double Crushed Nerve Damage
The term double crush syndrome (DCS) was coined by Harvard University plastic surgeons Albert Upton and Alan McComas, who wrote, “Neural function is impaired when compressed axons at one site cause the nerve to become especially susceptible to damage at another site” (Image 1.). Their double crush research began after observing that many carpal, cubital, and radial tunnel patients also complained of unilateral shoulder, chest, and upper back pain.1 While the DCS mechanism is not completely understood, it likely involves nerve sensitization and neuroplastic changes in the pain-modulating systems of the brain and spinal cord.
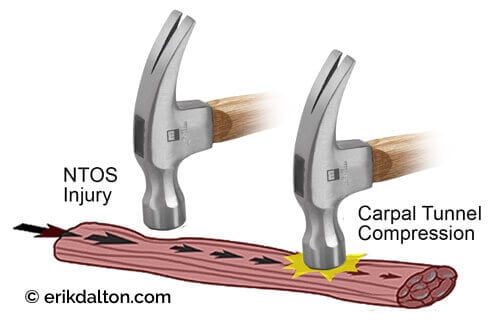
Neural compression of the brachial plexus is suitably called neurogenic thoracic outlet syndrome (NTOS). These clients present with a variety of symptoms, including painless atrophy of intrinsic hand muscles and nighttime paresthesia. Athletes may have difficulty grasping a racquet or ball, and some report pain. However, I’ve found that rather than being the main pain event, NTOS is more of an enhancer of symptoms at a distal site, such as the carpal tunnel. Put simply, the brain pays more attention to double crush nerve insults and is more likely to respond with pain or spasm.
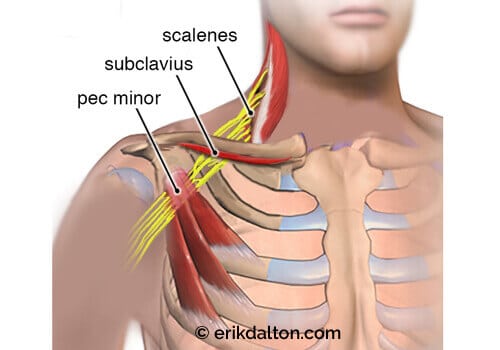
Although most clinicians feel that NTOS is an underestimated cause of DCS, assessment is often difficult due to vague, fluctuating symptoms. Instead of chasing the pain, I’ve achieved superior outcomes by palpating and releasing all fibrous connective tissue sites that may be kinking, stretching, or inflaming the brachial plexus. I address carpal and radial tunnel compression sites, then palpate and release NTOS contractures at the interscalene triangle, costoclavicular canal, and retropectoralis minor spaces (Image 2.).
Interscalene Impingement
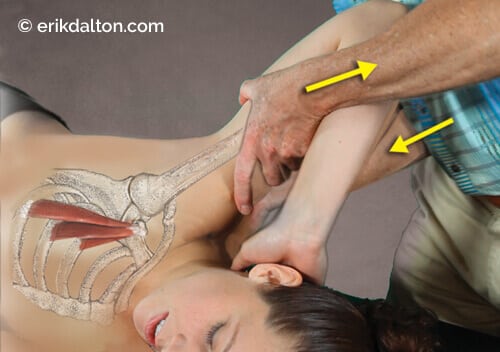
Nerve fibers originating at the spinal cord travel from the neck, through the thoracic outlet, and into the hand, providing sensation and movement during daily tasks. Certain postures or sleeping positions may increase tension and pressure on entrapped nerves. Further complicating the nerve’s journey through the thoracic outlet, researcher David B. Roos, MD, FACS, discovered irregular fibrous bands that increased brachial plexus stiffness and decreased movement.2 Roos classified 10 types of contractures that can stiffen the already unforgiving boundaries of the thoracic outlet container. Despite all the neural roadblocks, it has been my experience that many DCS clients respond well to massage, movement, and any type of cognitive training that lowers the brain’s threat level during movement. In Image 3., I demonstrate my favorite anterior and middle scalene stretch to create space at the interscalene triangle.

Subclavius and the Costoclavicular Canal
In clients with a drooping clavicle, the underlying subclavius muscle can reduce the costoclavicular canal size and compress the brachial plexus against the first rib. Upper chest breathing can exacerbate the problem, as the first rib elevates during inhalation and can get stuck there. A 2015 study published in BMC Research Notes also noted brachial compression from the subclavius posticus muscle, which ties the first rib to the superior border of the scapula.3 Rather than dig in to the sensitive tissues under the clavicle, I always begin with the subclavius stretch demonstrated in Image 4. This slow, gentle, graded exposure stretch is designed to reassure the brain that it’s now safe to move in previously painful positions.

Retropectoralis Muscle Impingement
Repetitive movements of the arms above the head, common among tennis enthusiasts, may cause friction and overstretch the nerve plexus under the pectoralis minor at the coracoid. The least irritating way I’ve found to create space here is by stretching the distal fibers that attach to ribs 3, 4, and 5. Notice in Image 5. that the stretch is directed at a 135-degree angle, which is the approximate pectoralis muscle fiber angle from coracoid to the rib insertions.
Many NTOS studies recommend postural correction, including muscle strengthening and lengthening for double crush complaints. However, there is no consensus in the literature as to exactly which muscles should be targeted. Posture is dynamic and the best results are gained through whole-body strengthening and balancing programs such as swimming, yoga, and martial arts. The bodywork goal is to bring mental awareness to areas of restriction and to teach the client it is safe to move through those previously painful barriers.
References
1. A. R. Upton and A. J. McComas, “The Double Crush in Nerve Entrapment Syndromes,” Lancet 2, no. 7825 (August 1973): 359–62.
2. D. B. Roos, “The Thoracic Outlet Syndrome is Underrated,” Archives of Neurology 47, no. 3 (1990): 327–28.
3. J. Muellner et al.,“Neurogenic Thoracic Outlet Syndrome Due to Subclavius Posticus Muscle with Dynamic Brachial Plexus Compression:A Case Report,” BMC Research Notes 8, no.351(August 2015).doi:10.1186/s13104-015-1317-3.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








