However, there does appear to be an innate wisdom that uses the nervous system as a conduit to transmit electrical impulses of intelligence to all the body’s systems that maintains mother and fetus in a state of homeostasis and balance. Regrettably, mechanical pressure on the central nervous system can interfere with the normal transmission of this vital intelligence. Since all of the mother’s systems and organs are now providing for two, it is obvious that optimal posture and functioning is critical for the baby’s healthy development.
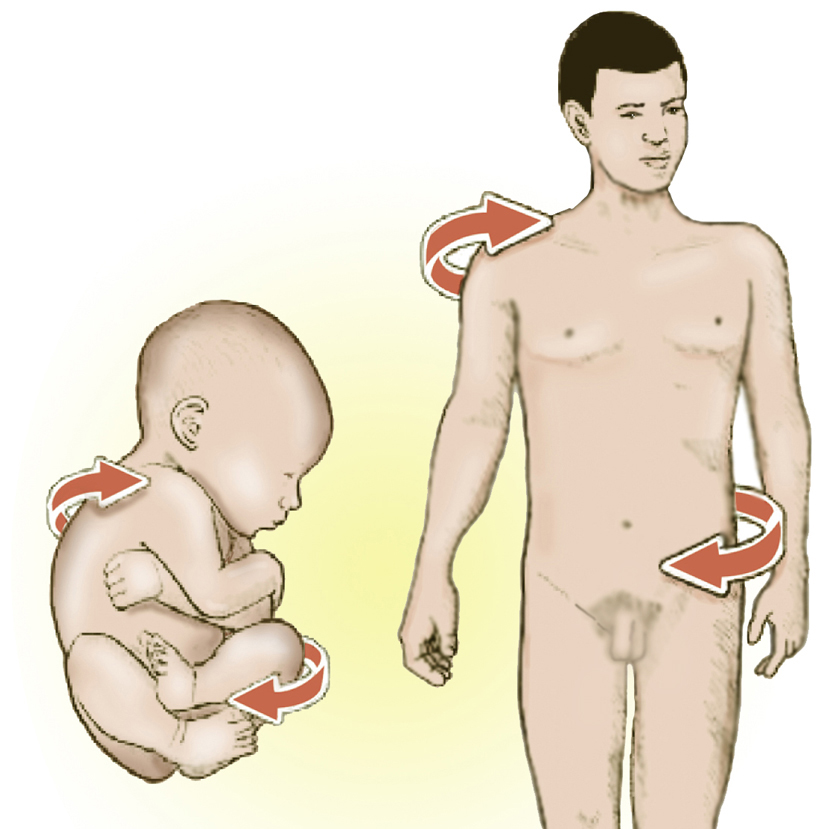
We begin our adventure into motherhood by introducing some very intriguing theories detailing how third trimester fetal positioning in momma’s womb may create aberrant adult postural patterns seen daily in our offices and clinics. Basic hands-on pelvic balancing and trunk stabilization routines taken from my Advanced Myoskeletal Techniques textbook are also included so therapists can aid expectant mothers in their quest for a healthy happy delivery. But before introducing the various postural theories and techniques, a brief overview of Mother Nature’s remarkable art of birthing requires thoughtful consideration.
Fetal Lie and Posture
Cerebral Lateralization
Structural Role of Pregnancy

Hey, Mom…it’s tight in here
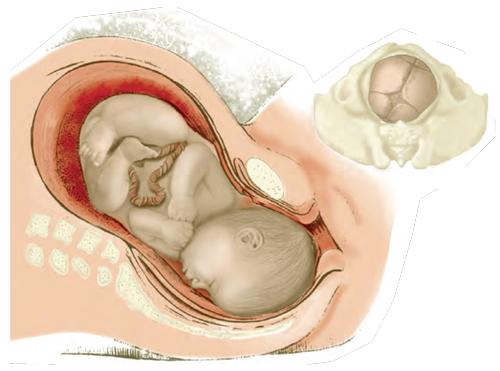
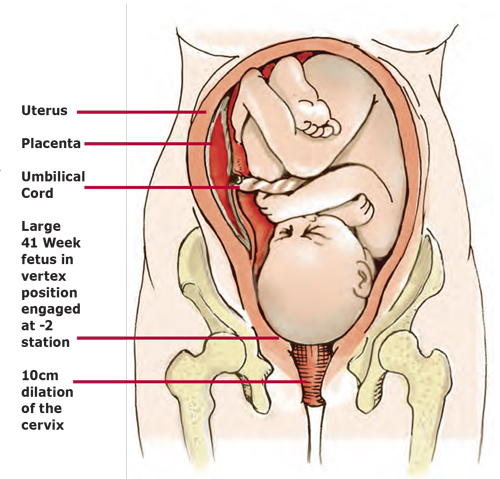
As space in mother’s womb becomes more compacted during the final trimester, the embryo’s arms and legs sometimes curl in various positions and occasionally the head finds itself stuck between the legs or “sunny-sideup” rather that turned to one side or the other. “Sunny-side-up” is the phrase assigned to babies whose heads have drifted from the normal flexed and rotated position into a backward-bent state of hyperextension. Today, more and more “sunny-side-up” presentations are showing up in hospitals around the world due to such things as:
- Poor posture.
- Mother prone to slouching in soft-cushioned furniture causing loss or reversal of normal lumbar lordotic curve;
- Weakened trunk stabilizers.
- Inadequate support in transversus abdominus, multifidus, obliques, and rectus abdominis.
- Lack of proper manual therapy.
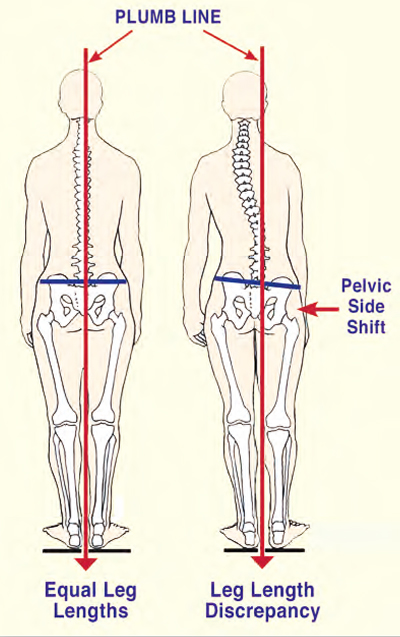
- Poor structural alignment before, during and after delivery, i.e., presence of aberrant upper and lower crossed patterns, spread rectus abdominis muscles, pelvic obliquity, etc.
Rectus Abdominis and Low-back Pain
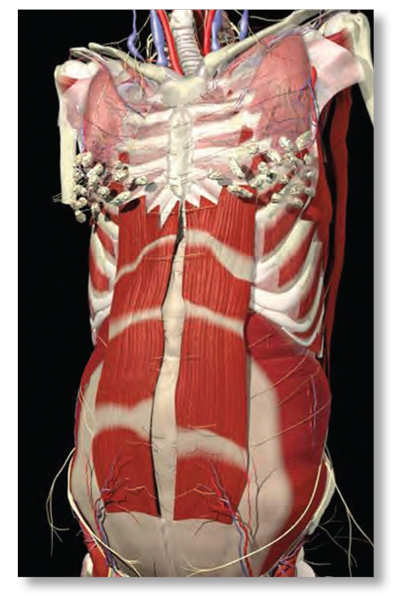
After a few sessions, the weakened abdominal support system “wakes up” as the recti regain muscle memory. With the recti muscles toned and back in the mid-line, the pubis and ribcage are pulled closer together which posteriorly rotates the pelvis and reciprocally reduces lumbar lordosis.
Ligamentous Support or Collapse
Provided the pelvis is in a balanced state, the ligamentous web attaching to the uterus maintains an equalized, supportive, antigravity suspension system. Any type of pelvic imbalance that causes the ligaments to become torqued and twisted, results in uterine constraint which limits the space available for the developing baby. At the least, any compromised position the baby must endure during pregnancy can have some sort of detrimental affect on his or her optimal development. Conditions such as torticollis are not uncommon in babies suffering uterine constraint.
If the shape of the woman’s uterus becomes distorted as birth approaches, the baby is prevented from getting into the best possible position for birthing. And even if the baby manages to place himself in the desirable head down position, a tight uterine cavity can prevent the baby’s head from moving into the ideal presentation for delivery. The head can become slightly tilted to one side or even more traumatically, present in the posterior position. Any fetal position that alters the baby’s correct habitus even slightly during birth will slow labor and add pain to both mother and baby. Women are often told that their babies were too big, or labor “just slowed down” when it was really the baby’s presentation interfering with the normal process and progression. Because excessive body weight tends to exaggerate ingrained aberrant postural patterns, therapists must address all soft tissues and osseous tissues (beginning with the feet) that may alter pelvic balance.
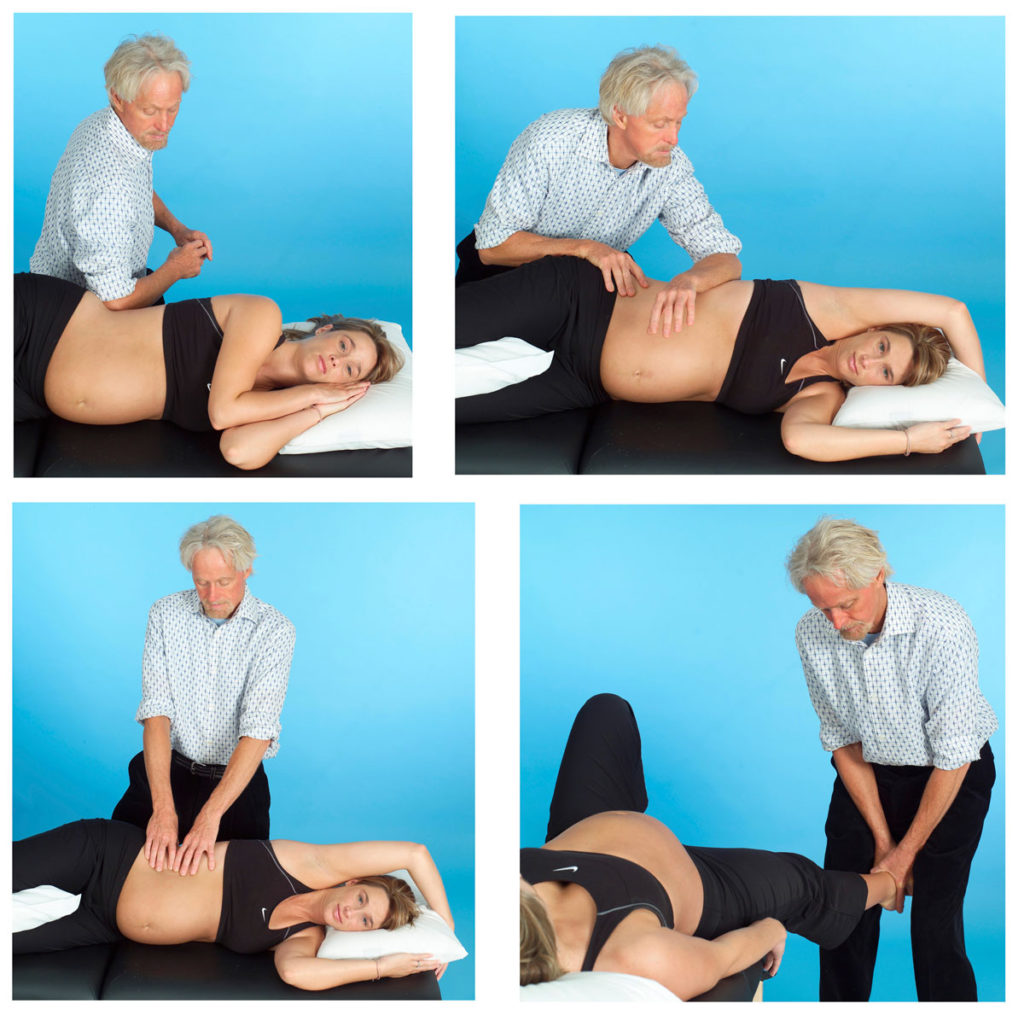
Mothers with a tendency for foot pronation and valgus knees are particularly susceptible to ligamentous laxity when the relaxin hormone enters the system during the third trimester. As the woman’s weight increases and medial ankle ligaments (spring and deltoid) become lax, the already pronated talus bone continues its medial glide off the calcaneus causing the foot and arch to drop into hyperpronation. Image 13. demonstrates a very therapeutic myoskeletal technique for bringing balance to a misaligned talocalcaneal joint due to weakened ankle ligaments. Recall that ligaments like stress but do not like strain. Ankle, knee, and pelvic alignment should be assessed and corrected during each session.
Homework
Home retraining exercises that focus on restoration of proper tone in the trunk stabilizers, diaphragms, and pelvic floor muscles are essential therapeutic pieces of the pregnancy puzzle. Transversus abdominis, pelvic-clock and Thera-Band toning routines boost therapeutic outcomes when performed on a regular basis between sessions. Pilates, yoga, Rolf Movement and other trunk stabilizing programs also seem effective in helping the body’s innate self-regulatory mechanisms produce a healthy happy baby.
Best Possible Scenario:
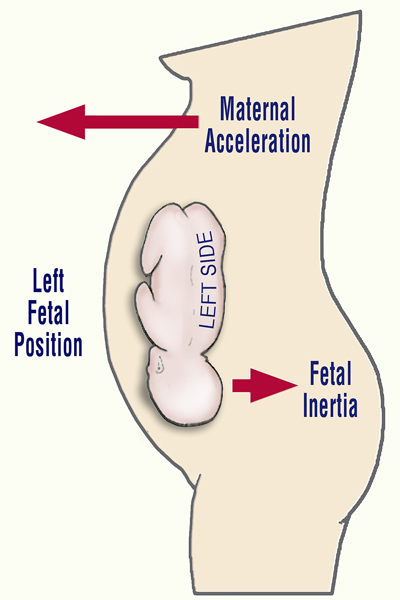
The mother’s best chance for a normal left fetal lie delivery requires that:
- No pelvic bowl asymmetries exist, i.e., sacroiliac, iliosacral, or side-shifted dysfunctions;
- Proper tone be present in the deep trunk stabilizers and lumbar multifidus;
- No spreading (past three fingers’ width) of the recti muscles at midline;
- Obstetrician or midwife directed therapeutic exercises be practiced regularly for adequate abdominal and trunk stabilization support.
These and other factors will not only help determine the habitus, presentation and delivery of the child, but will also play a major role in proper development and shape of the adult vertebral column. As stated above, early embryologic positioning often forms aberrant fascial rotational preferences that can become exaggerated during one’s lifetime due to life’s little micro and macro traumas. This compensatory process manifests as a loss of range of motion, tissue texture abnormalities (fascial contractures, fibrosis, etc.), and posturally initiated pain. During the final trimester, fascial restrictions can encumber proper blood and lymph flow and create neurological interferences that travel throughout all the body’s soft tissues. Fascial distortions frequently generate pressure gradient alterations in the thoracic outlet, respiratory, and pelvic diaphragms and are major contributors to stagnation in the vascular, lymphatic, endocrine, and respiratory systems. Myoskeletal Zone Therapy incorporates special techniques for eliminating stagnation by restoring optimal diaphragmatic function.
To help guarantee a successful and unremarkable delivery, the baby needs the maximum amount of space in the mother’s uterus and pelvis at exactly the time it is needed. The baby will make a very determined effort to achieve the correct position for birth, but can face resistance if a mother is unaware or unsure of her role in assisting the baby throughout the process. The third trimester of pregnancy, commencing at seven months gestational age, heralds the perinatal period. This critical stage is of greatest concern due to the propensity for adversity in the fetal presentation, position, and attitude.
The biomechanical implications affecting fetal well-being during the third trimester, and for the preparatory phase for labor and delivery, embrace any fetal alignment other than the optimal longitudinal lie, vertex presentation, and flexion attitude. Fetal positioning during the third trimester is not only crucial to an uneventful delivery but possibly to the final construction of the baby’s posture from adolescence through adulthood.
References
- R. Louis Schultz and Rosemary Feitis, The Endless Web: Fascial Anatomy and Physical Reality (Berkeley: North Atlantic Books, 1996).
- J. G. Zink, “Applications of the Osteopathic Holistic Approach to Homeostasis,” American Academy of Osteopathy Yearbook, (1973): 37-47.
- Fred H. Previc, “General Theory Concerning the Prenatal Origins of Cerebral Lateralization in Humans,” Psychological Review 98 (July 1991): 299-334.
- Ibid.
- S. R. Chhibber and I. Singh, “Asymmetry in Muscle Weight and One-sided Dominance in the Human Lower Limbs,” Journal of Anatomy 106 (1970): 553-556.
- M. Lacour, et al. “Spinal Effects of Electrical Vestibular Stimulation in
- Humans,” Acta Otolaryngologica 78 (1974): 399–409.
- B. Milojevic and J. Watson, “Vestibular Asymmetries in Right- and Left-handed People,” Acta Otolaryngologica 60 (1965): 322–330.
- R. J. von Baumgarten and R. Thumler, “A Model for Vestibular Function in Altered Gravitational States,” Life Sciences and Space Research 17 (1979):161-70.
- Previc, Psychological Review.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.